|
20/5/2022 0 Comments My clinic reflection dated April 2019: Following on from Compassion fatigue... Part 2My articles are not designed to replace medical advice. If you have an injury or other concerns I would recommend seeing a qualified health professional. The last time I posted was back in April 2019, it really has been a while! What with trying to live, work, continually study to progress professionally and personally, whilst trying please everyone in my life (work, boss, family, significant other and friends) but myself! Experiencing the loss of a loved ones, the pandemic, nearly dying from covid-19 myself, being redeployed and here I am, time really does fly… Mel Robins was right! No one cares (apart from your parents if you are lucky enough to have them in your life mine was my mother) and no one is coming, the only person who can rescue you is yourself! I KNOW and believe no -one will take better care of you then Allah (God, or whatever you have faith in) and yourself. 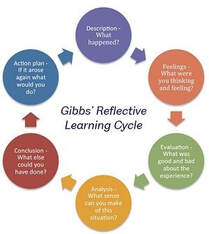 This piece was originally handwritten on the day in April 2019, the original plan was to write a reflective piece following the Gibbs Cycle of reflection see. The more time past the more I reflected on what’s been going on the more I realised I need to make sense of it all. I decided to write what I experienced, saw, understood and felt... in the words of Mayda Del Valle the poet “some days I feel geometric and go off on a tangent”. It was one of those days and exactly how I was feeling... I decided to rebel against the system and their rules “I am being non-compliant….” seen as physio's love to throw this word around. What the hell does not compliant mean anyhow (a blog for another day)! Of note it’s now 2022 and I am also sat here wondering why I didn’t upload this reflective piece when I wrote this in 2019. Then sat down on Friday 19th March 2021 at 6pm (I should of finished at 4:30pm) trying desperately finish off my endless notes, referrals, emails and calls to the patients and GPs. So I can complete this blog and post it! I wasn't brave enough to share this post and I am kind of still fearful if I am honest. Life, Procrastination and Perfectionism can be a b**** sometimes… Where am I going with this, (who knows, I have a lot to say and make sense of)? But I do know this, if you’re dealing with a bunch of baggage you didn’t know you was carrying. Start working in an uncaring environment driven by: labels, numbers, money, caring for other people’s wellbeing while work does not care about its staff wellbeing, can be disastrous. Don’t get me wrong life and work is not all doom and gloom and not everyone is bad, I have made a handful of fantastic lifelong friends along the way. I also learned a lot about; the world my place in it, myself, including my resilience for reflection and change and what it means to have the capacity to have this. I learned in order to change the system you have to conform to create reform, I gave this a shot it worked for a short while but I realised this isn’t really for me. So I decided to put my head down and do what you can here. Make every encounter you have with someone count, make it meaningful and positive. Be the change you wish to see in a world that, at times can be dark and full of despair. I also realised trying to help others means you need many things: boundaries, emotion regulation and so on. They definitely don’t teach this in school that’s for sure (in my experience). A lack of self awareness, boundaries and emotion regulation can be risky for instance: people pleasing can cause you to miss red flags if all you are focused on is trying to make the patient like you and help them. It’s actually unhelpful. This piece is for anyone who has struggled, may you find peace in knowing you are not alone everyone does struggle. As the stoics say life is suffering/ hard you just need to choose your, hard. I hope this information gives you the courage to: lean into the discomfort, know yourself, learn to say yes and when to say NO, stand your ground, be kind and true to who you are. Thank you for taking the time to read… So back to the topic of compassion fatigued continued / reflection / blog / mini rant This rant/ reflection/ blog whatever you would like to call it, may not necessary describe a particular event, but what it does describe is my frustrations, thoughts, difficulties and feelings about work, life and some of the pressure we (NHS) face on a daily basis.  What we are told and perceive to have “Lack of time” (I may touch on lack of resource also). One of the phases I constantly heard being thrown around was “are you managing your time appropriately” or my favourite, “lack of time” it really pisses me off. First of all time is a concept which is man-made and before the Big Bang there was no such thing as time according to the theory of relativity. In fact we have been conditioned to conform to a system which is governed by THEIR concept of time and what is dictated as a priority. Physicists, philosophers have often thought of as time being something “we experience time is psychologically real…. but time is not fundamentally real, they are artificial constructs/ perspectives of the human mind” Whether the concept of time or lack of time is real or not we all to some extend have been conditioned to conform to a system which is governed by others time and not our own…. I never started to work as a physiotherapist because I was worried about time I became a physiotherapist because I love making a meaningful difference to others. I am still to this day not sure how I became a physiotherapist. I remember doing my first year of my Sports Sciences degree at Brunel (2006) buying a jumper with the print at the back of the jumper saying physiotherapist instead of sports scientist (don’t ask me why I have no clue). Looking back perhaps I was manifesting this into existent without knowing… Other times I feel other influences have paved my way. Whatever the true jump start was, I know I thrive off helping. I have heard many describe health care professionals any things,
Despite having my own issues with vulnerability, I managed to mask how I felt, got lost in other people’s pain, because I found it easier to help others in need than deal with my own stuff (time & hindsight has given me this clarity). Having a natural predisposition to being; kind, helpful, and caring does help, I don’t like the idea of seeing anyone or anything suffer if something can be done. Helping others gives me a sense of purpose and meaning, it has also taught me perspective and gratitude. But I have realised without boundaries this can be risky, and unhealthy. I learned it’s a good thing to show signs of vulnerability. But what I didn’t know at the time was, you need to figure how who you can share this with (Brene Brown helped me make sense of this, you should check out the marble cup people), so I got burnt and learned this the hard way personally and professionally. I realised no one’s kindness is truly altruistic, most people’s kindness is transactional, YEP let that sink in for a hot minute. I know! Transactional kindness is a thing, some do it intentionally some do it unintentionally, I feel it links to Freud’s theory of secondary gain (more about this later) in a more lateral way rather than related to a particular illness. Helping others, self-sacrifice with no knowledge of what boundaries are and how to keep them is a dangerous thing! The problem with this (caring etc) in the context of working in the NHS means you yourself either suffer in order to maintain the standard you choose to have or you give up conform and fall in line, like the rest of them and eventually become empty. You keep getting told: be careful what you say, how you say it you don’t want to end up being “boxed ".In the field of health-care once you’re “in a box” it’s over, it’s harder to fit in or get the recognition or job promotion you’re after. I find this really odd, why do people feel the need to categorise you or put you in a box, just so they can label you? Are we all not striving for the same thing? The other thing I also hear often “we don’t have time”, although some say its not about money to a degree it is. In my old clinic we got paid per new client & NOT per contact, this would explain why we were pushed into seeing a lot of new patients (obviously don’t get me wrong people need to be seen, I understand this) & discharging fast. So how do you create time to give the care you wish to give? Also what kind of care is the best care? Creating time isn't easy...! Staying back late means not getting your time back or being paid for over time, it also means you are not recognised by your colleagues as being proactive or going above and beyond and exceeding expectations. Instead in this environment you are seen as “not managing your time and case load, the one who stays late”. Patients don’t realise this (why should they) but when a health care professional chooses to spend more time with you it’s not because you have time it’s because you have given up your time; your lunch break, giving up your admin time or choosing to see the next patient late. By choosing to do the above means you are staying back at work late going home late or go into work before your shift to complete necessary tasks (notes must be complete within 24 hours, legally). This reminds of the famous quote “you are free to choose but not free from the consequences of your choice”. I wonder when you weigh up all the options do you really have the freedom of choice or just the illusion? It is frustrating and overwhelming sometimes knowing your time is restricted because work (those who have never worked at grass routes level) feel 15-20 minutes is enough time to greet your patient, assess, educate, treat and have your hands washed, notes complete clinic room cleaned in time for your next patient. This is worse unfortunately for the GP’s their contact time is being reduced to 7 minutes per patient and each patient is only allowed to talk about one thing on each visit I understand if we spend less time with each of our contacts / patients this means more time for; cleaning, having the notes written up/ letters complete, more people will be seen. Because more people always need to be seen in the NHS. But at WHAT COST…… reduced time means mistakes can be more easily made, often this is sometimes certain things can be missed resulting in never event occurring. 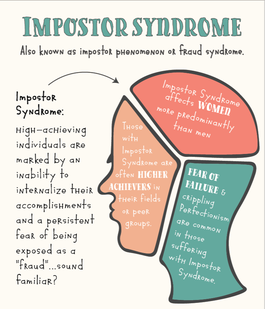 For those of you who do not know what imposter syndrome is, it is defined as “high achieving individuals who are marked by an inability to internalise their accomplishments and a persistent fear of being exposed as a “fraud”. Imposter syndrome cam develop when one “underestimates their own vales, skills, and accomplishments”. Apparently imposter syndrome is more commonly seen in college students, medical students and high level professionals. I guess this makes sense! I often feel undeserving of what I have achieved or I don’t recognise my accomplishments. I am aware my perfectionist and over achieving mentally or wanting to be good enough doesn’t help. I am also dyslexic and dyspraxic (neuro-divergent) so this does and doesn’t help, I need time to make sense of things and not make mistakes, I get cognitively more tired than most (long covid has made this worse) which is why having more time and space helps (which you often don’t get at work). Plus I like taking care of my clients/patients properly. Couple my own limitations (which I know I need to learn to keep in check) with working in an environment which is not nurturing will take its toll 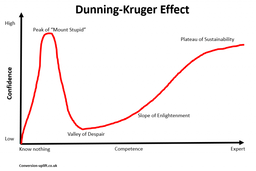 It also doesn’t help when you are compared to others and you are often told “others do it quicker finish earlier & on-time why can’t you…?” it makes me feel like I am a fraud like I don’t know enough or I have not done enough or even worse I am not enough. Feeling like an imposter or being a perfectionist can be good but also hindering (if it’s not kept in check) and it has its limitations. Just like those who act over confident like the already know everything, which is the other end of the spectrum and it’s called the Dunning –Kruger Effect, which is a common form of cognitive bias. I think being an over thinker is properly better than being so arrogant that you can’t recognise your own short comings / red flags “ignorance of ones ignorance”, but this is my own bias. The thing is what most don’t realise is, if this isn’t kept in check it can lead to burn out anxiety, depression, emotional exhaustion, low self-esteem and chronic stress. (Baumann et al). These adverse traits can lead to a decline in mental health, physical well-being, relationships, and work performance. Which I have definitely felt within myself. Having less time in my diary, no empty slots for time to do other tasks o decompressing, feels pressurising; it also feels like I am doing a disservice to my patients who have waited a long time to be seen. Reduced contact time makes it hard for me to connect in a meaningful way. A way where you can ensure you have created a safe, calm space so your patients feel what you have done resonates with them, they feel heard, happy and reassured when they leave. How do you build a strong bond/ therapeutic alliance with your patients? Whilst, knowing work dictates how long you should spend with someone (when you are meant to be an autonomous practitioner) and your diary is so full you barely have time to drink water because this would mean you need to create non-existent time to urinate…. It takes skill and time and involves many facets such as: - Active listening - Empathy - Friendliness - Encouragement - Confidence - No- verbal communication (open body language) - Patient education which is simple and clear - Knowledgeable therapist - Individualized treatment options - Taking patients opinions and preferences into consideration - Giving patients enough time for thorough assessment and management - Flexibility with patient appointments and care
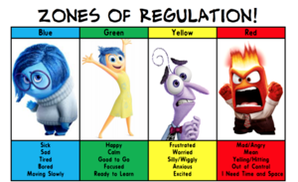
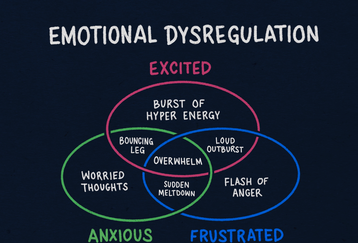
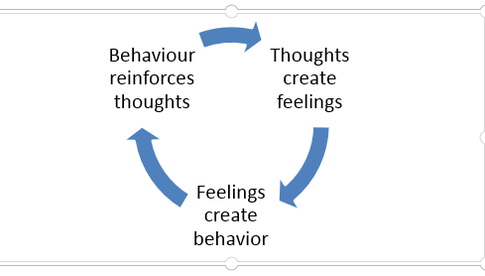
This means as a clinician you need to be regulated yourself to have the capacity to recognise when your patient isn’t and recognise that you will need to, stop “physio red flag screening” and be prepared to:
In order to decide if the person is right for you and if they are not, then where to sign post them next. This can be extremely hard, when work dictates how long you should spend with someone (when you are meant to be an autonomous practitioner) and your diary is so full you barely have time to drink water because this would mean you need to create non-existent time to urinate…. ! Why is emotion regulation important? |
| Lastly my favourite cut your treatment time down to 10-15 minutes so you can have time for yourself to complete necessary tasks….. Seriously….. I mean come on, you cannot squeeze blood out of a rock, and I know their heart is in the right place but how about cut me and the team some slack. Or give me a shit sandwich let me know what I am doing well on and what I could improve on rather than trying to make me fell like shit because I don’t fit into this magical box everyone else does. Many will choose to stay quiet don’t say anything because there is no point nothing will change and you might already rock a sinking ship. |
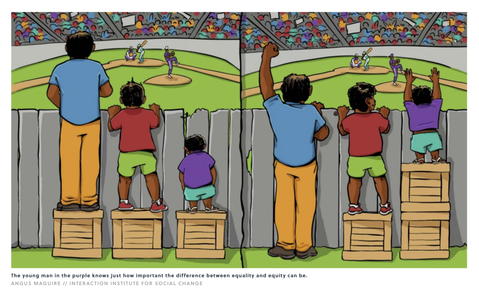
The fact is Rome was not built in a day and no, no one is the same and no one functions the same. But large cooperation’s will try to push you into a box calling this equality, diversity and inclusion. They seem to forget that Equality doesn’t mean you treat everyone the same and expect them to reproduce the same outcome.
Equality, fairness, inclusion diversity means so much more, it means getting to know your staffs needs, tailoring what support and training you provide them. Most importantly understand how to take care of your staff because not everyone will be able to produce the same output or function the way you want just because everyone else seems to be able to do it. Equality, diversity and inclusion and most importantly fairness in the workplace is multifaceted, and varies from one work place to the next. Take a look at this image for instance not everyone is the same but when they get treated the same inequality can still exist…
Equality, fairness, inclusion diversity means so much more, it means getting to know your staffs needs, tailoring what support and training you provide them. Most importantly understand how to take care of your staff because not everyone will be able to produce the same output or function the way you want just because everyone else seems to be able to do it. Equality, diversity and inclusion and most importantly fairness in the workplace is multifaceted, and varies from one work place to the next. Take a look at this image for instance not everyone is the same but when they get treated the same inequality can still exist…
| Anyways I have clearly digressed to far another topic for another day. As I was stating earlier the lack or limited time means you can not spend time unpacking your chronic/ complex/ persistent pain patient’s status and needs. Some of these types of individuals have no clue (not that its there fault, sometimes its just the way of the world)… They do not know what physiotherapy is, how physiotherapy can help them and what is has to offer. In my experience and from my own personal research I find these types of individuals really do need a clear explanation and sometimes this may mean on multiple occasions. They also need time to process what’s happened, what’s been said. They also need to feel heard and secure enough to be vulnerable to share their story and engage in their consultation / rehab. |
Extra time means you can pick up on clinical flags and decide how base to action these. Here are some examples of different types of flags;
• RED- signs of serious pathology
• ORANGE- psychiatric symptoms
• YELLOW- beliefs, appraisals and judgement , emotional responses, pain behaviours (including pain and coping strategies aka Capacity for resilience)
• BLUE- perceptions about the relationship between health and work
• BLACK- system or contextual obstacles
• Other - Expectations, function, Goals, Level of knowledge, and the list could go on.
Time allows health care professionals to help a patient build a short term secure base of attachment so that we are able to explore what is really meaningful to them. Sometimes this means giving reassurance, praise, care (love /affection) a high five when necessary. If none of the above can happen because we do not have time then it will really be difficulty to create tailored treatment plan/ intervention that is meaningful to the patient let alone a strong therapeutic alliance.
• RED- signs of serious pathology
• ORANGE- psychiatric symptoms
• YELLOW- beliefs, appraisals and judgement , emotional responses, pain behaviours (including pain and coping strategies aka Capacity for resilience)
• BLUE- perceptions about the relationship between health and work
• BLACK- system or contextual obstacles
• Other - Expectations, function, Goals, Level of knowledge, and the list could go on.
Time allows health care professionals to help a patient build a short term secure base of attachment so that we are able to explore what is really meaningful to them. Sometimes this means giving reassurance, praise, care (love /affection) a high five when necessary. If none of the above can happen because we do not have time then it will really be difficulty to create tailored treatment plan/ intervention that is meaningful to the patient let alone a strong therapeutic alliance.
In addition to this the more complex a case / person is the harder the challenge is to give the patient what they feel they want or need and what you feel they need. Because sometimes they don’t know and in actual fact what they think they want or need is nothing but a collection of thoughts, advice, ideas, recommendations, and beliefs from others.
This leads me onto what I experienced in the last couple of days/ weeks in my clinic when I had initially wrote this reflective piece:
• A mother who discussed committing suicide and asked me not to tell her pregnant daughter,
• A father who discussed how he plans to commit suicide after his daughters wedding day
• A mother who is so worried about her son she has lost the will to live
• A father who had to raise two children on his own because his wife left him for another man
• A woman who suffered years of emotional and physical abuse at the hands of her partner and now she has to watch her son lose his children because he has turned out to be an alcoholic.
• A mother whose son has become verbally and physically abusive to his brother, mother and father and how they live in fear
• A woman who was gunned down by the neighbour due to a blood feud that had nothing to do with her, now she is running for her life and is a refugee in a foreign country with no one to support her. She has lost the use of her leg and has a daughter who bullies her into not using her walking stick because she is embarrassed of how her mother looks.
This is just to list a few things I have had to hear and deal with.
For the first time I had to excuse a link worker without the patient realising and debrief the crying link worker as she could not handle what was said in the treatment room by the patient.
I had to ensure everyone wellbeing was taken care of, all of this whilst trying to keep my physiotherapy hat on to ensure I have done everything I should:
• Ensure there is no safe guarding risk
• Email the safe guarding lead – if unsure
• Deescalate the suicidal patient
• Call crisis team- because I have been unable to deescalate
• Call the GP notify him of their patients acute mental health crisis
• Write a letter regarding the acute mental health crisis or potential safe guarding issue
• Notify my senior in case I am off ill and someone needs to speak with me
What a tall order… lastly I then have to catch up with the other patients who expect to be seen but are now pissed that I am running late.
I have to ensure I don’t look upset and I am here to listen and help despite the fact that I may not have the mental capacity to do so… so what do you do as the British would say KEEP CALM AND CARRY ON….
This is one thing they do not teach you in school managing the above and then learning how not take this shit on broad and take it home. Like anything in life you either sink or swim and boy did I learn to swim….
This leads me onto what I experienced in the last couple of days/ weeks in my clinic when I had initially wrote this reflective piece:
• A mother who discussed committing suicide and asked me not to tell her pregnant daughter,
• A father who discussed how he plans to commit suicide after his daughters wedding day
• A mother who is so worried about her son she has lost the will to live
• A father who had to raise two children on his own because his wife left him for another man
• A woman who suffered years of emotional and physical abuse at the hands of her partner and now she has to watch her son lose his children because he has turned out to be an alcoholic.
• A mother whose son has become verbally and physically abusive to his brother, mother and father and how they live in fear
• A woman who was gunned down by the neighbour due to a blood feud that had nothing to do with her, now she is running for her life and is a refugee in a foreign country with no one to support her. She has lost the use of her leg and has a daughter who bullies her into not using her walking stick because she is embarrassed of how her mother looks.
This is just to list a few things I have had to hear and deal with.
For the first time I had to excuse a link worker without the patient realising and debrief the crying link worker as she could not handle what was said in the treatment room by the patient.
I had to ensure everyone wellbeing was taken care of, all of this whilst trying to keep my physiotherapy hat on to ensure I have done everything I should:
• Ensure there is no safe guarding risk
• Email the safe guarding lead – if unsure
• Deescalate the suicidal patient
• Call crisis team- because I have been unable to deescalate
• Call the GP notify him of their patients acute mental health crisis
• Write a letter regarding the acute mental health crisis or potential safe guarding issue
• Notify my senior in case I am off ill and someone needs to speak with me
What a tall order… lastly I then have to catch up with the other patients who expect to be seen but are now pissed that I am running late.
I have to ensure I don’t look upset and I am here to listen and help despite the fact that I may not have the mental capacity to do so… so what do you do as the British would say KEEP CALM AND CARRY ON….
This is one thing they do not teach you in school managing the above and then learning how not take this shit on broad and take it home. Like anything in life you either sink or swim and boy did I learn to swim….
0 Comments
Your comment will be posted after it is approved.
Leave a Reply.
Author
Sevda Onder
Nearly 20 years in the health and fitness industry.
Less than 10 years of post graduate physiotherapy experience.
£150 initial assessment
Physiotherapy 6/12 pack paid up front 15% off
Note I do offer low income slots for those who cannot afford my prices.
Please do not hesitate to reach out [email protected].
Less than 10 years of post graduate physiotherapy experience.
£150 initial assessment
Physiotherapy 6/12 pack paid up front 15% off
Note I do offer low income slots for those who cannot afford my prices.
Please do not hesitate to reach out [email protected].

 RSS Feed
RSS Feed