|
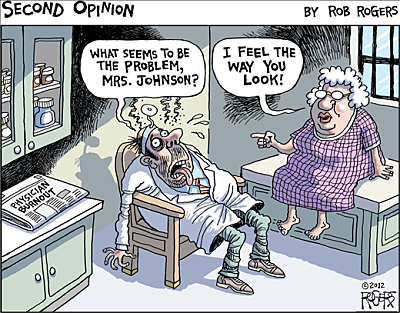
20/5/2022 0 Comments My clinic reflection dated April 2019: Following on from Compassion fatigue... Part 2My articles are not designed to replace medical advice. If you have an injury or other concerns I would recommend seeing a qualified health professional. The last time I posted was back in April 2019, it really has been a while! What with trying to live, work, continually study to progress professionally and personally, whilst trying please everyone in my life (work, boss, family, significant other and friends) but myself! Experiencing the loss of a loved ones, the pandemic, nearly dying from covid-19 myself, being redeployed and here I am, time really does fly… Mel Robins was right! No one cares (apart from your parents if you are lucky enough to have them in your life mine was my mother) and no one is coming, the only person who can rescue you is yourself! I KNOW and believe no -one will take better care of you then Allah (God, or whatever you have faith in) and yourself. 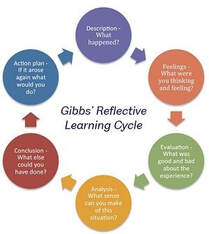 This piece was originally handwritten on the day in April 2019, the original plan was to write a reflective piece following the Gibbs Cycle of reflection see. The more time past the more I reflected on what’s been going on the more I realised I need to make sense of it all. I decided to write what I experienced, saw, understood and felt... in the words of Mayda Del Valle the poet “some days I feel geometric and go off on a tangent”. It was one of those days and exactly how I was feeling... I decided to rebel against the system and their rules “I am being non-compliant….” seen as physio's love to throw this word around. What the hell does not compliant mean anyhow (a blog for another day)! Of note it’s now 2022 and I am also sat here wondering why I didn’t upload this reflective piece when I wrote this in 2019. Then sat down on Friday 19th March 2021 at 6pm (I should of finished at 4:30pm) trying desperately finish off my endless notes, referrals, emails and calls to the patients and GPs. So I can complete this blog and post it! I wasn't brave enough to share this post and I am kind of still fearful if I am honest. Life, Procrastination and Perfectionism can be a b**** sometimes… Where am I going with this, (who knows, I have a lot to say and make sense of)? But I do know this, if you’re dealing with a bunch of baggage you didn’t know you was carrying. Start working in an uncaring environment driven by: labels, numbers, money, caring for other people’s wellbeing while work does not care about its staff wellbeing, can be disastrous. Don’t get me wrong life and work is not all doom and gloom and not everyone is bad, I have made a handful of fantastic lifelong friends along the way. I also learned a lot about; the world my place in it, myself, including my resilience for reflection and change and what it means to have the capacity to have this. I learned in order to change the system you have to conform to create reform, I gave this a shot it worked for a short while but I realised this isn’t really for me. So I decided to put my head down and do what you can here. Make every encounter you have with someone count, make it meaningful and positive. Be the change you wish to see in a world that, at times can be dark and full of despair. I also realised trying to help others means you need many things: boundaries, emotion regulation and so on. They definitely don’t teach this in school that’s for sure (in my experience). A lack of self awareness, boundaries and emotion regulation can be risky for instance: people pleasing can cause you to miss red flags if all you are focused on is trying to make the patient like you and help them. It’s actually unhelpful. This piece is for anyone who has struggled, may you find peace in knowing you are not alone everyone does struggle. As the stoics say life is suffering/ hard you just need to choose your, hard. I hope this information gives you the courage to: lean into the discomfort, know yourself, learn to say yes and when to say NO, stand your ground, be kind and true to who you are. Thank you for taking the time to read… So back to the topic of compassion fatigued continued / reflection / blog / mini rant This rant/ reflection/ blog whatever you would like to call it, may not necessary describe a particular event, but what it does describe is my frustrations, thoughts, difficulties and feelings about work, life and some of the pressure we (NHS) face on a daily basis.  What we are told and perceive to have “Lack of time” (I may touch on lack of resource also). One of the phases I constantly heard being thrown around was “are you managing your time appropriately” or my favourite, “lack of time” it really pisses me off. First of all time is a concept which is man-made and before the Big Bang there was no such thing as time according to the theory of relativity. In fact we have been conditioned to conform to a system which is governed by THEIR concept of time and what is dictated as a priority. Physicists, philosophers have often thought of as time being something “we experience time is psychologically real…. but time is not fundamentally real, they are artificial constructs/ perspectives of the human mind” Whether the concept of time or lack of time is real or not we all to some extend have been conditioned to conform to a system which is governed by others time and not our own…. I never started to work as a physiotherapist because I was worried about time I became a physiotherapist because I love making a meaningful difference to others. I am still to this day not sure how I became a physiotherapist. I remember doing my first year of my Sports Sciences degree at Brunel (2006) buying a jumper with the print at the back of the jumper saying physiotherapist instead of sports scientist (don’t ask me why I have no clue). Looking back perhaps I was manifesting this into existent without knowing… Other times I feel other influences have paved my way. Whatever the true jump start was, I know I thrive off helping. I have heard many describe health care professionals any things,
Despite having my own issues with vulnerability, I managed to mask how I felt, got lost in other people’s pain, because I found it easier to help others in need than deal with my own stuff (time & hindsight has given me this clarity). Having a natural predisposition to being; kind, helpful, and caring does help, I don’t like the idea of seeing anyone or anything suffer if something can be done. Helping others gives me a sense of purpose and meaning, it has also taught me perspective and gratitude. But I have realised without boundaries this can be risky, and unhealthy. I learned it’s a good thing to show signs of vulnerability. But what I didn’t know at the time was, you need to figure how who you can share this with (Brene Brown helped me make sense of this, you should check out the marble cup people), so I got burnt and learned this the hard way personally and professionally. I realised no one’s kindness is truly altruistic, most people’s kindness is transactional, YEP let that sink in for a hot minute. I know! Transactional kindness is a thing, some do it intentionally some do it unintentionally, I feel it links to Freud’s theory of secondary gain (more about this later) in a more lateral way rather than related to a particular illness. Helping others, self-sacrifice with no knowledge of what boundaries are and how to keep them is a dangerous thing! The problem with this (caring etc) in the context of working in the NHS means you yourself either suffer in order to maintain the standard you choose to have or you give up conform and fall in line, like the rest of them and eventually become empty. You keep getting told: be careful what you say, how you say it you don’t want to end up being “boxed ".In the field of health-care once you’re “in a box” it’s over, it’s harder to fit in or get the recognition or job promotion you’re after. I find this really odd, why do people feel the need to categorise you or put you in a box, just so they can label you? Are we all not striving for the same thing? The other thing I also hear often “we don’t have time”, although some say its not about money to a degree it is. In my old clinic we got paid per new client & NOT per contact, this would explain why we were pushed into seeing a lot of new patients (obviously don’t get me wrong people need to be seen, I understand this) & discharging fast. So how do you create time to give the care you wish to give? Also what kind of care is the best care? Creating time isn't easy...! Staying back late means not getting your time back or being paid for over time, it also means you are not recognised by your colleagues as being proactive or going above and beyond and exceeding expectations. Instead in this environment you are seen as “not managing your time and case load, the one who stays late”. Patients don’t realise this (why should they) but when a health care professional chooses to spend more time with you it’s not because you have time it’s because you have given up your time; your lunch break, giving up your admin time or choosing to see the next patient late. By choosing to do the above means you are staying back at work late going home late or go into work before your shift to complete necessary tasks (notes must be complete within 24 hours, legally). This reminds of the famous quote “you are free to choose but not free from the consequences of your choice”. I wonder when you weigh up all the options do you really have the freedom of choice or just the illusion? It is frustrating and overwhelming sometimes knowing your time is restricted because work (those who have never worked at grass routes level) feel 15-20 minutes is enough time to greet your patient, assess, educate, treat and have your hands washed, notes complete clinic room cleaned in time for your next patient. This is worse unfortunately for the GP’s their contact time is being reduced to 7 minutes per patient and each patient is only allowed to talk about one thing on each visit I understand if we spend less time with each of our contacts / patients this means more time for; cleaning, having the notes written up/ letters complete, more people will be seen. Because more people always need to be seen in the NHS. But at WHAT COST…… reduced time means mistakes can be more easily made, often this is sometimes certain things can be missed resulting in never event occurring. 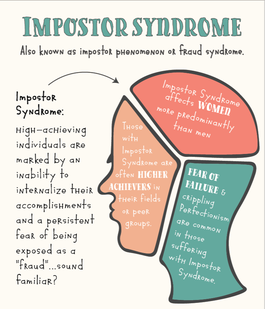 For those of you who do not know what imposter syndrome is, it is defined as “high achieving individuals who are marked by an inability to internalise their accomplishments and a persistent fear of being exposed as a “fraud”. Imposter syndrome cam develop when one “underestimates their own vales, skills, and accomplishments”. Apparently imposter syndrome is more commonly seen in college students, medical students and high level professionals. I guess this makes sense! I often feel undeserving of what I have achieved or I don’t recognise my accomplishments. I am aware my perfectionist and over achieving mentally or wanting to be good enough doesn’t help. I am also dyslexic and dyspraxic (neuro-divergent) so this does and doesn’t help, I need time to make sense of things and not make mistakes, I get cognitively more tired than most (long covid has made this worse) which is why having more time and space helps (which you often don’t get at work). Plus I like taking care of my clients/patients properly. Couple my own limitations (which I know I need to learn to keep in check) with working in an environment which is not nurturing will take its toll 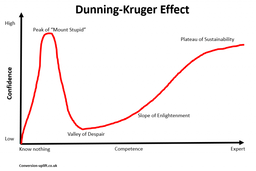 It also doesn’t help when you are compared to others and you are often told “others do it quicker finish earlier & on-time why can’t you…?” it makes me feel like I am a fraud like I don’t know enough or I have not done enough or even worse I am not enough. Feeling like an imposter or being a perfectionist can be good but also hindering (if it’s not kept in check) and it has its limitations. Just like those who act over confident like the already know everything, which is the other end of the spectrum and it’s called the Dunning –Kruger Effect, which is a common form of cognitive bias. I think being an over thinker is properly better than being so arrogant that you can’t recognise your own short comings / red flags “ignorance of ones ignorance”, but this is my own bias. The thing is what most don’t realise is, if this isn’t kept in check it can lead to burn out anxiety, depression, emotional exhaustion, low self-esteem and chronic stress. (Baumann et al). These adverse traits can lead to a decline in mental health, physical well-being, relationships, and work performance. Which I have definitely felt within myself. Having less time in my diary, no empty slots for time to do other tasks o decompressing, feels pressurising; it also feels like I am doing a disservice to my patients who have waited a long time to be seen. Reduced contact time makes it hard for me to connect in a meaningful way. A way where you can ensure you have created a safe, calm space so your patients feel what you have done resonates with them, they feel heard, happy and reassured when they leave. How do you build a strong bond/ therapeutic alliance with your patients? Whilst, knowing work dictates how long you should spend with someone (when you are meant to be an autonomous practitioner) and your diary is so full you barely have time to drink water because this would mean you need to create non-existent time to urinate…. It takes skill and time and involves many facets such as: - Active listening - Empathy - Friendliness - Encouragement - Confidence - No- verbal communication (open body language) - Patient education which is simple and clear - Knowledgeable therapist - Individualized treatment options - Taking patients opinions and preferences into consideration - Giving patients enough time for thorough assessment and management - Flexibility with patient appointments and care
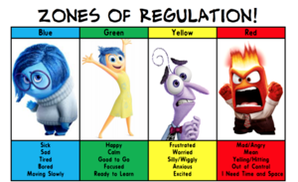
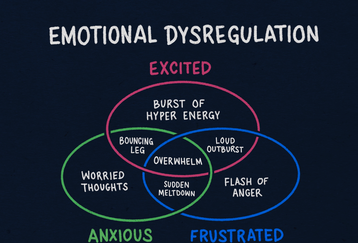
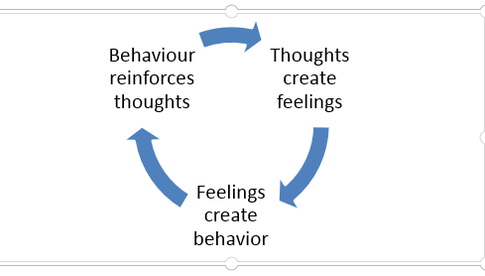
This means as a clinician you need to be regulated yourself to have the capacity to recognise when your patient isn’t and recognise that you will need to, stop “physio red flag screening” and be prepared to:
In order to decide if the person is right for you and if they are not, then where to sign post them next. This can be extremely hard, when work dictates how long you should spend with someone (when you are meant to be an autonomous practitioner) and your diary is so full you barely have time to drink water because this would mean you need to create non-existent time to urinate…. ! Why is emotion regulation important? |
| Lastly my favourite cut your treatment time down to 10-15 minutes so you can have time for yourself to complete necessary tasks….. Seriously….. I mean come on, you cannot squeeze blood out of a rock, and I know their heart is in the right place but how about cut me and the team some slack. Or give me a shit sandwich let me know what I am doing well on and what I could improve on rather than trying to make me fell like shit because I don’t fit into this magical box everyone else does. Many will choose to stay quiet don’t say anything because there is no point nothing will change and you might already rock a sinking ship. |
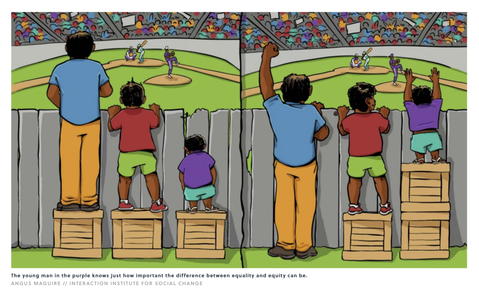
The fact is Rome was not built in a day and no, no one is the same and no one functions the same. But large cooperation’s will try to push you into a box calling this equality, diversity and inclusion. They seem to forget that Equality doesn’t mean you treat everyone the same and expect them to reproduce the same outcome.
Equality, fairness, inclusion diversity means so much more, it means getting to know your staffs needs, tailoring what support and training you provide them. Most importantly understand how to take care of your staff because not everyone will be able to produce the same output or function the way you want just because everyone else seems to be able to do it. Equality, diversity and inclusion and most importantly fairness in the workplace is multifaceted, and varies from one work place to the next. Take a look at this image for instance not everyone is the same but when they get treated the same inequality can still exist…
Equality, fairness, inclusion diversity means so much more, it means getting to know your staffs needs, tailoring what support and training you provide them. Most importantly understand how to take care of your staff because not everyone will be able to produce the same output or function the way you want just because everyone else seems to be able to do it. Equality, diversity and inclusion and most importantly fairness in the workplace is multifaceted, and varies from one work place to the next. Take a look at this image for instance not everyone is the same but when they get treated the same inequality can still exist…
| Anyways I have clearly digressed to far another topic for another day. As I was stating earlier the lack or limited time means you can not spend time unpacking your chronic/ complex/ persistent pain patient’s status and needs. Some of these types of individuals have no clue (not that its there fault, sometimes its just the way of the world)… They do not know what physiotherapy is, how physiotherapy can help them and what is has to offer. In my experience and from my own personal research I find these types of individuals really do need a clear explanation and sometimes this may mean on multiple occasions. They also need time to process what’s happened, what’s been said. They also need to feel heard and secure enough to be vulnerable to share their story and engage in their consultation / rehab. |
Extra time means you can pick up on clinical flags and decide how base to action these. Here are some examples of different types of flags;
• RED- signs of serious pathology
• ORANGE- psychiatric symptoms
• YELLOW- beliefs, appraisals and judgement , emotional responses, pain behaviours (including pain and coping strategies aka Capacity for resilience)
• BLUE- perceptions about the relationship between health and work
• BLACK- system or contextual obstacles
• Other - Expectations, function, Goals, Level of knowledge, and the list could go on.
Time allows health care professionals to help a patient build a short term secure base of attachment so that we are able to explore what is really meaningful to them. Sometimes this means giving reassurance, praise, care (love /affection) a high five when necessary. If none of the above can happen because we do not have time then it will really be difficulty to create tailored treatment plan/ intervention that is meaningful to the patient let alone a strong therapeutic alliance.
• RED- signs of serious pathology
• ORANGE- psychiatric symptoms
• YELLOW- beliefs, appraisals and judgement , emotional responses, pain behaviours (including pain and coping strategies aka Capacity for resilience)
• BLUE- perceptions about the relationship between health and work
• BLACK- system or contextual obstacles
• Other - Expectations, function, Goals, Level of knowledge, and the list could go on.
Time allows health care professionals to help a patient build a short term secure base of attachment so that we are able to explore what is really meaningful to them. Sometimes this means giving reassurance, praise, care (love /affection) a high five when necessary. If none of the above can happen because we do not have time then it will really be difficulty to create tailored treatment plan/ intervention that is meaningful to the patient let alone a strong therapeutic alliance.
In addition to this the more complex a case / person is the harder the challenge is to give the patient what they feel they want or need and what you feel they need. Because sometimes they don’t know and in actual fact what they think they want or need is nothing but a collection of thoughts, advice, ideas, recommendations, and beliefs from others.
This leads me onto what I experienced in the last couple of days/ weeks in my clinic when I had initially wrote this reflective piece:
• A mother who discussed committing suicide and asked me not to tell her pregnant daughter,
• A father who discussed how he plans to commit suicide after his daughters wedding day
• A mother who is so worried about her son she has lost the will to live
• A father who had to raise two children on his own because his wife left him for another man
• A woman who suffered years of emotional and physical abuse at the hands of her partner and now she has to watch her son lose his children because he has turned out to be an alcoholic.
• A mother whose son has become verbally and physically abusive to his brother, mother and father and how they live in fear
• A woman who was gunned down by the neighbour due to a blood feud that had nothing to do with her, now she is running for her life and is a refugee in a foreign country with no one to support her. She has lost the use of her leg and has a daughter who bullies her into not using her walking stick because she is embarrassed of how her mother looks.
This is just to list a few things I have had to hear and deal with.
For the first time I had to excuse a link worker without the patient realising and debrief the crying link worker as she could not handle what was said in the treatment room by the patient.
I had to ensure everyone wellbeing was taken care of, all of this whilst trying to keep my physiotherapy hat on to ensure I have done everything I should:
• Ensure there is no safe guarding risk
• Email the safe guarding lead – if unsure
• Deescalate the suicidal patient
• Call crisis team- because I have been unable to deescalate
• Call the GP notify him of their patients acute mental health crisis
• Write a letter regarding the acute mental health crisis or potential safe guarding issue
• Notify my senior in case I am off ill and someone needs to speak with me
What a tall order… lastly I then have to catch up with the other patients who expect to be seen but are now pissed that I am running late.
I have to ensure I don’t look upset and I am here to listen and help despite the fact that I may not have the mental capacity to do so… so what do you do as the British would say KEEP CALM AND CARRY ON….
This is one thing they do not teach you in school managing the above and then learning how not take this shit on broad and take it home. Like anything in life you either sink or swim and boy did I learn to swim….
This leads me onto what I experienced in the last couple of days/ weeks in my clinic when I had initially wrote this reflective piece:
• A mother who discussed committing suicide and asked me not to tell her pregnant daughter,
• A father who discussed how he plans to commit suicide after his daughters wedding day
• A mother who is so worried about her son she has lost the will to live
• A father who had to raise two children on his own because his wife left him for another man
• A woman who suffered years of emotional and physical abuse at the hands of her partner and now she has to watch her son lose his children because he has turned out to be an alcoholic.
• A mother whose son has become verbally and physically abusive to his brother, mother and father and how they live in fear
• A woman who was gunned down by the neighbour due to a blood feud that had nothing to do with her, now she is running for her life and is a refugee in a foreign country with no one to support her. She has lost the use of her leg and has a daughter who bullies her into not using her walking stick because she is embarrassed of how her mother looks.
This is just to list a few things I have had to hear and deal with.
For the first time I had to excuse a link worker without the patient realising and debrief the crying link worker as she could not handle what was said in the treatment room by the patient.
I had to ensure everyone wellbeing was taken care of, all of this whilst trying to keep my physiotherapy hat on to ensure I have done everything I should:
• Ensure there is no safe guarding risk
• Email the safe guarding lead – if unsure
• Deescalate the suicidal patient
• Call crisis team- because I have been unable to deescalate
• Call the GP notify him of their patients acute mental health crisis
• Write a letter regarding the acute mental health crisis or potential safe guarding issue
• Notify my senior in case I am off ill and someone needs to speak with me
What a tall order… lastly I then have to catch up with the other patients who expect to be seen but are now pissed that I am running late.
I have to ensure I don’t look upset and I am here to listen and help despite the fact that I may not have the mental capacity to do so… so what do you do as the British would say KEEP CALM AND CARRY ON….
This is one thing they do not teach you in school managing the above and then learning how not take this shit on broad and take it home. Like anything in life you either sink or swim and boy did I learn to swim….
0 Comments
Nothing is ever what it seems
My youngest memory of myself has always been me caring for someone and something, at the time I did not comprehend how powerful or debilitating being constantly compassionate, caring empathetic can be. I remember basing many of my decisions especially becoming a physiotherapist on this super power. I wanted to make a positive impact on a persons life. I chose to give because I wanted to and because I had the capacity too. What I did not realise when you enter a career that involves someone else having authority over your time on; what you give, how much you give coupled with a large complex case load, never ending tasks, poor or limited recourses and so much little time to complete them in., that it can lead to;
If you had told me as a student being in a giving job could cause you to suffer this I would of said shut the front door why could doing what I love cause me so much pain. Little did I know the first person(s) or thing to teach you about love is also the first thing/ person(s) to teach you about pain.
The term burnout according to many can be understood as a collection of symptoms which include;
Much to my surprise this is more common in women then in men, although I wonder whether this is because its under reported. It turns out being a more experience physiotherapist may also put you at a greater risk of developing compassion fatigue, I also wonder whether this is because of mileage and longer exposure to an unforgiving fast paced work environment. I have to admit at some points in my career I have definitely felt a state of emotional exhaustion due to intensive empathic involvement with people who were or are in distress.
When I look back, I did not once remember being taught to be; aware, recognise and or leans to manage clinical burnout. I was so preoccupied after graduation from university feeling unprepared and rushing to get myself up to scratch. Which is very common almost all under grads who graduate feel like they know nothing. The is is usually heighten when you become land your first role as a fresh junior band 5. I remember being thrown into a VERY busy MSK clinic, which felt like I was being put through the conveyor belt. Not only are you expected to know everything (all knowing all seeing god),but you are also expected to have your whole initial assessment complete within 30-40 minutes max, hands washed, diagnosis, prognosis, treatment plan explained, taught and your notes written up in a timely fashion. Because your next patient is already sitting in the waiting room waiting to be seen by you. You then rush to grab the notes from the new patient draw introduce yourself and observe your patient walking down the corridor while you rush to read the notes (try and figure out asap what the hell they are here for and start thinking of what your diagnosis could be). All this should be done while trying not to looked stressed out and rushed off your feet.
My youngest memory of myself has always been me caring for someone and something, at the time I did not comprehend how powerful or debilitating being constantly compassionate, caring empathetic can be. I remember basing many of my decisions especially becoming a physiotherapist on this super power. I wanted to make a positive impact on a persons life. I chose to give because I wanted to and because I had the capacity too. What I did not realise when you enter a career that involves someone else having authority over your time on; what you give, how much you give coupled with a large complex case load, never ending tasks, poor or limited recourses and so much little time to complete them in., that it can lead to;
- Clinical Burnout
- Compassion/ Empathy Fatigue
- Burnout Syndrome
- Moral Distress
- Occupational burnout
- Secondary Traumatic Stress Syndrome (STSS)
If you had told me as a student being in a giving job could cause you to suffer this I would of said shut the front door why could doing what I love cause me so much pain. Little did I know the first person(s) or thing to teach you about love is also the first thing/ person(s) to teach you about pain.
The term burnout according to many can be understood as a collection of symptoms which include;
- Mental, Physical and the less spoken about Emotional exhaustion
- Stressed
- Insomnia
- Anxiety
- Low mood some might even feel depressed
- Low immune system aka a vulnerability to illness and the list could go on
Much to my surprise this is more common in women then in men, although I wonder whether this is because its under reported. It turns out being a more experience physiotherapist may also put you at a greater risk of developing compassion fatigue, I also wonder whether this is because of mileage and longer exposure to an unforgiving fast paced work environment. I have to admit at some points in my career I have definitely felt a state of emotional exhaustion due to intensive empathic involvement with people who were or are in distress.
When I look back, I did not once remember being taught to be; aware, recognise and or leans to manage clinical burnout. I was so preoccupied after graduation from university feeling unprepared and rushing to get myself up to scratch. Which is very common almost all under grads who graduate feel like they know nothing. The is is usually heighten when you become land your first role as a fresh junior band 5. I remember being thrown into a VERY busy MSK clinic, which felt like I was being put through the conveyor belt. Not only are you expected to know everything (all knowing all seeing god),but you are also expected to have your whole initial assessment complete within 30-40 minutes max, hands washed, diagnosis, prognosis, treatment plan explained, taught and your notes written up in a timely fashion. Because your next patient is already sitting in the waiting room waiting to be seen by you. You then rush to grab the notes from the new patient draw introduce yourself and observe your patient walking down the corridor while you rush to read the notes (try and figure out asap what the hell they are here for and start thinking of what your diagnosis could be). All this should be done while trying not to looked stressed out and rushed off your feet.
This concept is well documented, known and understood by many yet no mention of this topic at university, or by your colleagues. Until YES you've guessed it when you start showing signs of cracking.
Their are various challenges with inpatient and outpatient work. But I have to admit outpatients msk I have found to be the most rewarding but also the most mentally, physically and emotionally labouring / draining.
I believe one of the reasons I experienced bur out is partially due to nature and circumstance. Since I can remember I’ve been a carer for my nan and now my mum, it was only natural I that I should end up in a caring role. In addition to this because I care and sometimes self doubt myself I will tend to DO ALL MY I’S AND CROSS MY T’S. What might some might not consider as MSK remit and a falls assessment for instance as non msk. I would consider as patient centered care and as a must especially if they are a falls risk. As a health care professional that works in the NHS we all know how much it costs the NHS should a person’s fall and require treatment. But I also know how significantly traumatising and most often life altering fracture due to a fall can be. I also know how long it takes to get someone who is a falls risk unit a falls prevtion group. So every patient/ client I encounter I see them as someone’s mum, nan, dad, brother, sister. I will endeavour to go above and beyond, because If someone I cared for ended up requiring care then I would want them to also be treated well.
However this kind of work ethic is a double edged sword beucase you need to care to do your job and do it well. What it also means, is this kind of work ethic and characteristic can either be a concoction for beautiful story or a complete disaster.
I believe one of the reasons I experienced bur out is partially due to nature and circumstance. Since I can remember I’ve been a carer for my nan and now my mum, it was only natural I that I should end up in a caring role. In addition to this because I care and sometimes self doubt myself I will tend to DO ALL MY I’S AND CROSS MY T’S. What might some might not consider as MSK remit and a falls assessment for instance as non msk. I would consider as patient centered care and as a must especially if they are a falls risk. As a health care professional that works in the NHS we all know how much it costs the NHS should a person’s fall and require treatment. But I also know how significantly traumatising and most often life altering fracture due to a fall can be. I also know how long it takes to get someone who is a falls risk unit a falls prevtion group. So every patient/ client I encounter I see them as someone’s mum, nan, dad, brother, sister. I will endeavour to go above and beyond, because If someone I cared for ended up requiring care then I would want them to also be treated well.
However this kind of work ethic is a double edged sword beucase you need to care to do your job and do it well. What it also means, is this kind of work ethic and characteristic can either be a concoction for beautiful story or a complete disaster.
13/4/2019 1 Comment
My reflection in October 2016: Non-specific lower back pain in Women’s health: Musculoskeletal masqueraders ...
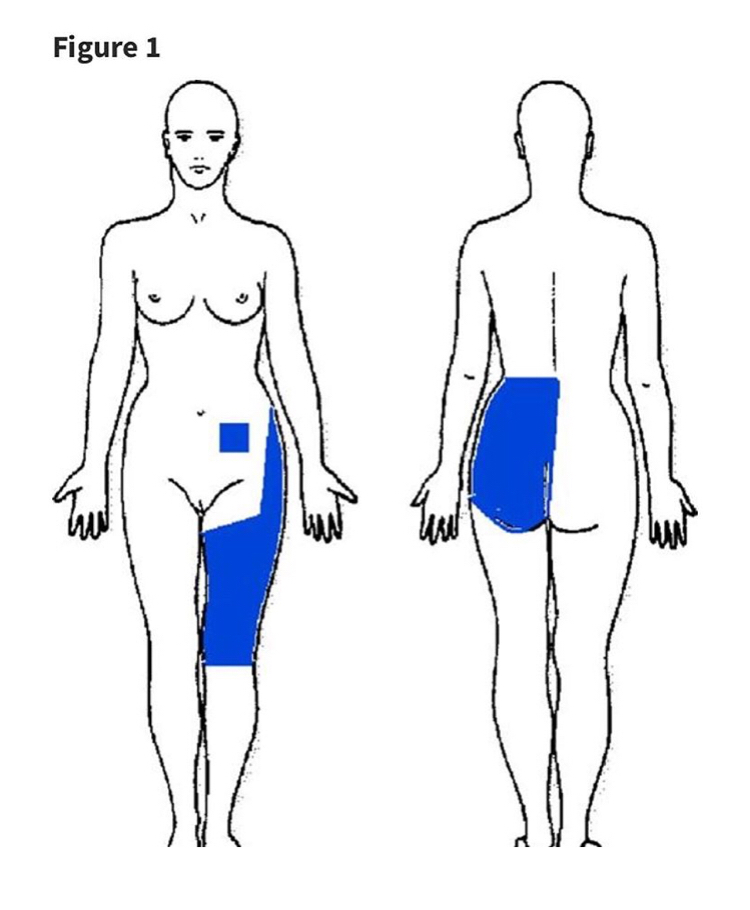
Figure 1 is from the article link is attached below in the article
Nothing is NEVER what it seems extraxt from Troyer (2007) Differential Diagnosis of Endometriosis in a Young Adult Woman With Nonspecific Low Back Pain!
When you see a 25-year-old female with 5 year Hx (history) on and off pain with sudden onset of severe left-sided lumbo-sacral, lower quadrant, buttock, and thigh pain.
She had pain on flexion and prolonged walking or sitting.
No eases
Disturbed sleep & awoken with pain
Bowels -NAD (nothing abnormally denoted)
Bladder last 2 years Increased urgency and frequency
Objective examination (O/E)
reduced flexion with pain EOR (end of range) extension was clear.
Power 4/5 for Bilat Lower limbs
Reduced sensation
Passive straight leg raise (PSLR) did not reproduce her leg pain only back pain,
Reflexes KJ & AJ both bilaterally present
Full passive range of motion (ROM) at the Hip
Negative Patrick's test.
Low BMI (body mass index)
Investigations -
MRI of lumbar NAD (nothing abnormally denoted)
Urine analysis negative for infections
Family Hx
Strong Family Hx RA (rheumatoid arthritis) and hypothyroidism
Result
Turns out the nonspecific or mechanical low back pain is NOT THE PAIN DRIVER, this young lay had Endometriosis and left sided ovarian cyst....
You learn something new EVERYDAY!
For those that do not know endometriosis is, it is a COMMON gynaecological disorder in women between 25-30 and can mimic musculoskeletal symptoms and manifest as nonspecific low back pain. This is why you should always be thinking outside the box, because nothing is ever what it seems. Not ever patient who turns up at your door step will have MSK issues as the MAIN PAIN DRIVER (which I will be doing a reflection on another reflection/blog). Definitely a useful and one remember when you are deferentially diagnosing a patient :)
Article:
Troyer (2007) Differential Diagnosis of Endometriosis in a Young Adult Woman With Nonspecific Low Back Pain. Physical Therapy, Volume 87, Issue 6, 1 June 2007, Pages 801–810,
Link: https://academic.oup.com/ptj/article/87/6/801/2747261
Update- January 2019
When I read this article it later came in handy when I came across a patient who actually presented with something very similar. We are currently working on their MSK issues - whilst they are being investigated to rule out other possible causes such as:
Update- March 2019
They have been discharged from my care to continue managing their MSK low back pain with a graded exercise program and to stay under the care of gynecology for further management of their ovarian cyst and fibroid's.
When you see a 25-year-old female with 5 year Hx (history) on and off pain with sudden onset of severe left-sided lumbo-sacral, lower quadrant, buttock, and thigh pain.
She had pain on flexion and prolonged walking or sitting.
No eases
Disturbed sleep & awoken with pain
Bowels -NAD (nothing abnormally denoted)
Bladder last 2 years Increased urgency and frequency
Objective examination (O/E)
reduced flexion with pain EOR (end of range) extension was clear.
Power 4/5 for Bilat Lower limbs
Reduced sensation
Passive straight leg raise (PSLR) did not reproduce her leg pain only back pain,
Reflexes KJ & AJ both bilaterally present
Full passive range of motion (ROM) at the Hip
Negative Patrick's test.
Low BMI (body mass index)
Investigations -
MRI of lumbar NAD (nothing abnormally denoted)
Urine analysis negative for infections
Family Hx
Strong Family Hx RA (rheumatoid arthritis) and hypothyroidism
Result
Turns out the nonspecific or mechanical low back pain is NOT THE PAIN DRIVER, this young lay had Endometriosis and left sided ovarian cyst....
You learn something new EVERYDAY!
For those that do not know endometriosis is, it is a COMMON gynaecological disorder in women between 25-30 and can mimic musculoskeletal symptoms and manifest as nonspecific low back pain. This is why you should always be thinking outside the box, because nothing is ever what it seems. Not ever patient who turns up at your door step will have MSK issues as the MAIN PAIN DRIVER (which I will be doing a reflection on another reflection/blog). Definitely a useful and one remember when you are deferentially diagnosing a patient :)
Article:
Troyer (2007) Differential Diagnosis of Endometriosis in a Young Adult Woman With Nonspecific Low Back Pain. Physical Therapy, Volume 87, Issue 6, 1 June 2007, Pages 801–810,
Link: https://academic.oup.com/ptj/article/87/6/801/2747261
Update- January 2019
When I read this article it later came in handy when I came across a patient who actually presented with something very similar. We are currently working on their MSK issues - whilst they are being investigated to rule out other possible causes such as:
- Ovarian cyst
- Fibroid's
- Endometriosis
Update- March 2019
They have been discharged from my care to continue managing their MSK low back pain with a graded exercise program and to stay under the care of gynecology for further management of their ovarian cyst and fibroid's.
27/10/2018 0 Comments
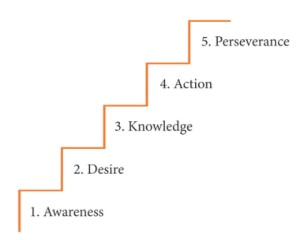
Random thoughts, readings and ramblings of a geeky therapist: Enabling behaviour change check list
Behaviour change checklist to follow for anyone who is involved in dealing with patients/ clients.
This is in no specific order:
Understand what motivates people
Remember
This is in no specific order:
- Identify where they are at now
- What have they tried before, what happened?
- What do they believe they want?
- What is their learning style
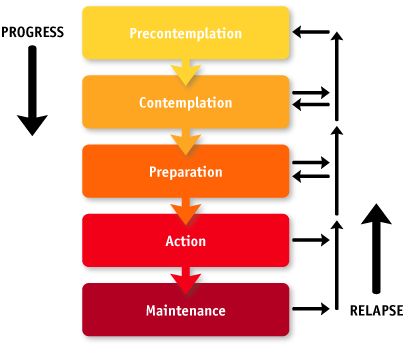
- Identify what stage of readiness your client/ patient is at?. If you don't know start to probe so you can figure this out!
- Getting a client to take responsibility for their own health is essential ask probing questions
- Identify what their confidence level is on a scale of 0-10
- What will support they need in order to be more confident and in more control
- What are they consequences if they do not make the change now
- What are the consequences if they do change
- When coaching your client / patient you must focus on coaching them and not giving advice as advising only builds RESISTANCE to change
- Coaching means believing there is always a solution to every problem
- Coaching means their is no such thing as failure only FEED BACK
- YOU as a therapist/ coach must take responsibility for your communication with your client and the meaning they put on it. If it doesn't work CHANGE IT
- To be a good coach you must believe the solution to your clients problem is inside of them
- Ideally teach your client to fish for themselves not give them the fish!!!
- Never forget if they have come to you and they are at a stage of action. Set appropriate goals to help take the from action to maintenance stage.
- Remember it takes 6 months or slightly more before your patient / client will move into the maintenance stage.
- Do not forget it is very easy for people to slip back into their old habits from maintenance stage. Especially during times of high stress
- Teach them to learn what their triggers are and how to be confident in self managing their set backs/ relapses or flare ups
- If you are a personal trainer arrange weekly or monthly coaching calls. If you are physio arrange your follow up appointments accordingly. This is to help keep your client in check and remind them of their why and re- focus them.
Understand what motivates people
- People are motivated from moving away from pain and into pleasure
- When you are coaching your patients/ clients you should always ask your clients to focus on their goals and how their life will be different if they achieved them (moving into pleasure)
- What does their choice mean? Does it have an end or beginning? For example Lance Armstrong had a beginning he won the Tour de France after he was diagnosed with gesticulate cancer because that diagnosis gave him a new meaning to his life. He increased his emotional and psychological fitness!
- Avoid making your clients dwell on how they are now it can bring them down
- Remind your clients “The more rules they have about how they should be, the less happy your clients are going to be happy". - Tony Robbins
- Help move your patients/ clients out of the mindset that we are our past... If they live with that mind set then your past is your future.
- Remind them were their is a will their is a way, your circumstances are NOT the defining factor!!!
- The defining factor is never lack of resources it’s how resourceful you are
- Remind your patient/ client that their emotion is a resource. If you are able to coach them to focus their emotion and energy into one area in their life and attach the right type of meaning to it. This will give your client a sense of purpose.
- Success does not happen over night, the journey is more important then the summit
- Teach your clients that their choice shape their destiny
- Rituals define us... What you do to achieve your physique is defined by the rituals you set in place everyday!
- Daily rituals help build a stronger focus, foundation and which will enable them to attain their goal
- Teach your client to surround themselves with those who they look up to and can compete with on a healthy level
Remember
- For many (patients/ clients) being out of there comfort zone is the biggest stumbling block to success. So how do you make it easy for them to succeed? What plan of action can you put in place?
- Change is uncomfortable and many perceive that the change they have to apply to their lifestyle is greater than their current pain
- Change will only occur when the desire to change is greater than their resistance to change
- Your job as a therapist/ coach / personal trainer is to manage that uncomfortable period and reduce the resistance to change
References
Les Brown (1998) It’s Not Over Until You Win: How To Become the Person You Have Always Wanted To Be, No Matter What the Obstacle
Mike Williams (2008) The Road To Your Best Stuff: Taking Your Career, Business or Cause to the Next Level and Beyond
Paul Chek (2014) Embracing The Change Process Part 1 to Part 5, YouTube video
Tony Robbins (2001) Awaken the Giant Within: How to Take Immediate Control of Your Mental, Emotional, Physical and Financial Life
Les Brown (1998) It’s Not Over Until You Win: How To Become the Person You Have Always Wanted To Be, No Matter What the Obstacle
Mike Williams (2008) The Road To Your Best Stuff: Taking Your Career, Business or Cause to the Next Level and Beyond
Paul Chek (2014) Embracing The Change Process Part 1 to Part 5, YouTube video
Tony Robbins (2001) Awaken the Giant Within: How to Take Immediate Control of Your Mental, Emotional, Physical and Financial Life
14/1/2016 1 Comment
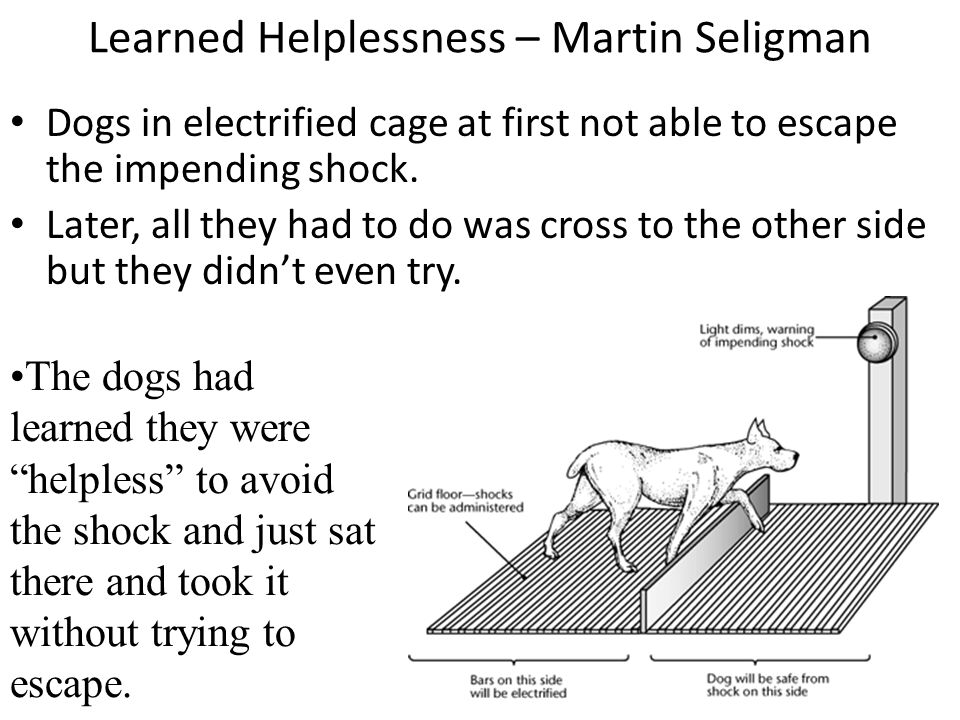
Random, thoughts, readings and ramblings of a geeky therapist part 2: Learned Helplessness
You made it to part 2 😁 thank you for coming back.
So by now you should have some kind of understanding of what we do and why we are the way we are....
There are multiple factors that contribute to the way we respond and the way we are. This doesn’t necessary mean it’s a bad thing it just means how you are, what you do and how you or your client/patient has coped thus far has served a purpose. It’s got you or your client/ patient safely to this point, and now it may no longer be serving you.
Remember, there is so much more to life than just training to look good etc. It’s about finding out your why, what does this mean to you. When you know yours or your clients/patients why then it becomes easier to find the right strategy to break those OLD hard wired patterns and instil new ones. More often than not as a coach, personal trainer, therapist we also need to recognise our own bias, triggers, thoughts, patterns and beliefs break them and learn to keep them in check.
It is important if you are seeking change you need to find someone who cares and has your best interests at heart. It is also important as a therapist, coach or trainer to screen your patient, client appropriately and understand where they are and what they need.
I guess what I am saying is in order to deal with patients / clients it is important to be equipped with more than just knowledge on exercise prescription for example treating low back pain or deal with weight loss or gain.
I believe the missing link between each scenario boils down to many factors below is just a short list:
If you are your client, patient is not changing perhaps you need to go back and re-valuate your screening process. If you do not have:
For example let's consider the concept of learned helplessness.
Learned helplessness is a phenomenon which was discovered in the 1967 by an American psychologist called Martin Seligman who conducted the controlled study, which was later expanded by Seligman and others. The dogs were exposed to repeated bouts of electric shocks who attempted to leave the cage they were in. When the dogs were unable to escape or avoid the painful experience, they quickly learned they were unable to control the situation and learned be helpless.
There are multiple factors that contribute to the way we respond and the way we are. This doesn’t necessary mean it’s a bad thing it just means how you are, what you do and how you or your client/patient has coped thus far has served a purpose. It’s got you or your client/ patient safely to this point, and now it may no longer be serving you.
Remember, there is so much more to life than just training to look good etc. It’s about finding out your why, what does this mean to you. When you know yours or your clients/patients why then it becomes easier to find the right strategy to break those OLD hard wired patterns and instil new ones. More often than not as a coach, personal trainer, therapist we also need to recognise our own bias, triggers, thoughts, patterns and beliefs break them and learn to keep them in check.
It is important if you are seeking change you need to find someone who cares and has your best interests at heart. It is also important as a therapist, coach or trainer to screen your patient, client appropriately and understand where they are and what they need.
I guess what I am saying is in order to deal with patients / clients it is important to be equipped with more than just knowledge on exercise prescription for example treating low back pain or deal with weight loss or gain.
I believe the missing link between each scenario boils down to many factors below is just a short list:
- Attachment trauma- see John Bowlby for further information
- Learned helplessness
- Fear of failure
- Low self-esteem and or confidence
- Shame and or guilt
- A sense of unworthiness
- Overwhelmed
- No support system in place
If you are your client, patient is not changing perhaps you need to go back and re-valuate your screening process. If you do not have:
- A good understanding of your client or yourself
- You are not sure what stage of readiness you or they are at
- You are not sure of what your own or their expectations are
- If you haven’t appropriately set realistic meaningful goals for yourself or them
For example let's consider the concept of learned helplessness.
Learned helplessness is a phenomenon which was discovered in the 1967 by an American psychologist called Martin Seligman who conducted the controlled study, which was later expanded by Seligman and others. The dogs were exposed to repeated bouts of electric shocks who attempted to leave the cage they were in. When the dogs were unable to escape or avoid the painful experience, they quickly learned they were unable to control the situation and learned be helpless.
How do dogs apply to humans? In its simplest terms when a person is exposed to repeated bouts of stress and they begin to feel a sense of loss, impending doom and helplessness.
A person’s resilience will begin to waiver and they will quickly realise that they are unable to control what’s going on, unfortunately the only choice they see they are able to make is to learn to stop trying and give up. What makes it worse is the majority of the population even in this day and age shy away from admitting that they are stressed, lost or in need of emotional support and guidance. The acceptance is that’s life and you just learn to deal, the sad truth is as a result of this kind of attitude many will go on to suffer chronic long term stress related disorders such as reduced resilience, depression and anxiety. This is because their personal beliefs, attitudes and perceived absence of over control over the outcome of the situation they are in.
Even with today's level of communication through advances in technology and free instant access to information that can help enhance our knowledge. It has still not been filtered down into mainstream society that those which are not nurtured or guided properly to understand how to deal with the uncontrollable stress life has to offer.
They have learned from past traumatic experiences, (previous attempts at rescuing one’s self) that no matter what nothing will change no matter what one does, so giving up is inevitable, “I might as well stop now or not even bother trying, what’s the point right? It hasn’t worked before and will not work now”. In fact repeated bouts of acute stress if not dealt with appropriately will have a negative physical and psychological effect on a person’s quality of life and wellbeing.
Is there a solution for this HELL YES, the vast amount of studies that have been conducted looking at the positive effects of exercise have all shown that exercise does help prevent the development of stress related mood disorders like depression and anxiety (Greenwood & Fleshner et al 2008). How and why well exercise actually increases the expression of a wide range of trophic factors throughout the brain, which are mediated by a large variety of neural and hormonal factors. In fact repeated consistent bouts of exercise actually helps produce anti-depressant effects especially with those who suffer from chronic depression.
But hold on a minute, if studies have found that exercise is the way forward to beat depression along with better nutrition positive thinking and sleep. Then why are we not all doing exercising more? Or why am I still unhappy even tho I do exercise? Well this could be for a number of reasons, Seligman study also found that it took roughly 25 times to drag the dogs across the lower barrier away from the electric shocks into the pain free zone before the dogs themselves learned that there is a way out.
A person’s resilience will begin to waiver and they will quickly realise that they are unable to control what’s going on, unfortunately the only choice they see they are able to make is to learn to stop trying and give up. What makes it worse is the majority of the population even in this day and age shy away from admitting that they are stressed, lost or in need of emotional support and guidance. The acceptance is that’s life and you just learn to deal, the sad truth is as a result of this kind of attitude many will go on to suffer chronic long term stress related disorders such as reduced resilience, depression and anxiety. This is because their personal beliefs, attitudes and perceived absence of over control over the outcome of the situation they are in.
Even with today's level of communication through advances in technology and free instant access to information that can help enhance our knowledge. It has still not been filtered down into mainstream society that those which are not nurtured or guided properly to understand how to deal with the uncontrollable stress life has to offer.
They have learned from past traumatic experiences, (previous attempts at rescuing one’s self) that no matter what nothing will change no matter what one does, so giving up is inevitable, “I might as well stop now or not even bother trying, what’s the point right? It hasn’t worked before and will not work now”. In fact repeated bouts of acute stress if not dealt with appropriately will have a negative physical and psychological effect on a person’s quality of life and wellbeing.
Is there a solution for this HELL YES, the vast amount of studies that have been conducted looking at the positive effects of exercise have all shown that exercise does help prevent the development of stress related mood disorders like depression and anxiety (Greenwood & Fleshner et al 2008). How and why well exercise actually increases the expression of a wide range of trophic factors throughout the brain, which are mediated by a large variety of neural and hormonal factors. In fact repeated consistent bouts of exercise actually helps produce anti-depressant effects especially with those who suffer from chronic depression.
But hold on a minute, if studies have found that exercise is the way forward to beat depression along with better nutrition positive thinking and sleep. Then why are we not all doing exercising more? Or why am I still unhappy even tho I do exercise? Well this could be for a number of reasons, Seligman study also found that it took roughly 25 times to drag the dogs across the lower barrier away from the electric shocks into the pain free zone before the dogs themselves learned that there is a way out.
What does this mean, to us?
Recognising from early on what expectations they have and traits your clients carry, will help allow you to formulate a plan that’s suited to them with a real WHY attached to why they must be consistent with the protocol you have provided.
This doesn’t mean it will always work but if you are able to recognise this as a coach, trainer and or therapist the above then I am 100% sure you have a plan B to then tackle why you, or your client / patient is falling off the band wagon. Remember, if as a coach/ trainer/therapist you are honest and authentic and show that you care with your clients will see this. No matter how bumpy the road maybe everything will fall into place if the time is right and the lesson has been learned.
Recognising from early on what expectations they have and traits your clients carry, will help allow you to formulate a plan that’s suited to them with a real WHY attached to why they must be consistent with the protocol you have provided.
This doesn’t mean it will always work but if you are able to recognise this as a coach, trainer and or therapist the above then I am 100% sure you have a plan B to then tackle why you, or your client / patient is falling off the band wagon. Remember, if as a coach/ trainer/therapist you are honest and authentic and show that you care with your clients will see this. No matter how bumpy the road maybe everything will fall into place if the time is right and the lesson has been learned.
29/12/2015 2 Comments
Random thoughts, readings and ramblings of a geeky therapist part 1: Learned Helplessness
I have always wondered what has stopped us from getting to where we want to be: life, work,
love and physically.
Scary moment... my first ever blog hopefully one of many! I hope you enjoy the read :)
In my short life span I have met some amazing, compassionate, driven and caring people. Who have enriched my life but yet are unable to recognise the greatness that they have within them. You know the ones I am talking about, their mere presence is oozing with uplifting energy, selfless / endless care and compassion. I have also noticed that these same people at one point or another some if not all did not know how to practice:
Seeing this made me genuinely wonder why, where did this type of behaviour stem from. Why do we behave in this manner.
It saddens me to see this kind of behaviour because I know first hand what poor self care, self love and not having the ability to regconise your own boundaries and say no.
I have also noticed that many and including myself tend to disguise our decisions based on the socially constructed concept of being “realistic”. When in fact I believe choosing to use this “I’m being realistic” term is just another way of sugar coating or denying perhaps what you truly feel about yourself. This is known as your self fulfilling prophecy or also your deep core belief.
If your mental chitter chatter often sounds like this:
Then be rest assured if you have been telling yourself this then your core belief about yourself is what could be holding you back from as Elliott Hulse would say “the best stronger version of your self”
Over time I have noticed the same story takes on many different shapes and forms, you may come across a client who is projecting this story onto you or you are projecting your story onto others about “being realistic”. When in reality if we stopped to understand what we are really feeling we would realise that perhaps our inner child hasn’t had their needs met as a child. These childhood traumas or wounds are what could be causing us to be resistant to change. This resistant to change most often comes from fear of:
I am concerned with this subject matter because it astounds me how many children walk around in an adults body still hurt and who have not healed from the wounds of their past. They walk around never knowing who they really are or understanding how they really feel, the term “walking dead” comes to mind.
This negative core belief you or they have about lthemselves, coupled with unhealed wounds and fear has perplexed if not all, many from achieving their true passion, purpose and potential in life.
In my short life span I have met some amazing, compassionate, driven and caring people. Who have enriched my life but yet are unable to recognise the greatness that they have within them. You know the ones I am talking about, their mere presence is oozing with uplifting energy, selfless / endless care and compassion. I have also noticed that these same people at one point or another some if not all did not know how to practice:
- The word no
- Self love
- Self care
- Energy conservation
Seeing this made me genuinely wonder why, where did this type of behaviour stem from. Why do we behave in this manner.
It saddens me to see this kind of behaviour because I know first hand what poor self care, self love and not having the ability to regconise your own boundaries and say no.
I have also noticed that many and including myself tend to disguise our decisions based on the socially constructed concept of being “realistic”. When in fact I believe choosing to use this “I’m being realistic” term is just another way of sugar coating or denying perhaps what you truly feel about yourself. This is known as your self fulfilling prophecy or also your deep core belief.
If your mental chitter chatter often sounds like this:
- What’s the point
- I’m a failure always have been
- Nothing will change it hasn’t before
- Or complete denial I don’t have a problem
- If it’s not broke don’t fix it
- I don’t need to change
Then be rest assured if you have been telling yourself this then your core belief about yourself is what could be holding you back from as Elliott Hulse would say “the best stronger version of your self”
Over time I have noticed the same story takes on many different shapes and forms, you may come across a client who is projecting this story onto you or you are projecting your story onto others about “being realistic”. When in reality if we stopped to understand what we are really feeling we would realise that perhaps our inner child hasn’t had their needs met as a child. These childhood traumas or wounds are what could be causing us to be resistant to change. This resistant to change most often comes from fear of:
- Loss
- Separation
- Abandonment
- Rejection
- Hurt or disappointed
- Being unworthy
- Unloveable and the list could go on.
I am concerned with this subject matter because it astounds me how many children walk around in an adults body still hurt and who have not healed from the wounds of their past. They walk around never knowing who they really are or understanding how they really feel, the term “walking dead” comes to mind.
This negative core belief you or they have about lthemselves, coupled with unhealed wounds and fear has perplexed if not all, many from achieving their true passion, purpose and potential in life.
Les Brown says it beautifully ”If you are not willing to risk, you can’t grow and if you can’t grow you can’t become your best and if you can’t become your best, you can’t be happy and if you can’t be happy, well what else will is there?”
I have also wondered when you or a person finally makes the steps to seek help, take action and make a change, more often then not there is a also a disconnect between a:
Why is it at times have we been unable to make a deeper lasting profound connection and bridge this gap.I mean it’s that simple right go to see a;
- Doctor an a patient
- Patient and a doctor
- Physiotherapist/ Osteopath and a patient
- Patient and physiotherapist / osteopath
- Personal trainer and a client
- Client and personal trainer
- Family and friends and so on and so on...
Why is it at times have we been unable to make a deeper lasting profound connection and bridge this gap.I mean it’s that simple right go to see a;
- Physiotherapist do your exercises and you will get better
- See a doctor get a pill it will get better
- See a therapist talk about how you feel this will help you get better
- See a personal trainer they will help you move better
- Workout what you want
- Now figure out how to set a goal
- Figure out how to break it down into to small short term, medium goals to achieve your long term goal
- Figure out how to stay motivated after the mood is long gone
- Don’t forget to be an adult and learn how to do your taxes and manage your finances
- Look after your health
- Learn how to cook
- Learn how to eat a well balanced meal (fats, carbs, protein, don’t forget your micro-nutrients)
- Eat all your meals
- Exercise 3 to 4 times a week
- Work a 40-60 hour week
- Don’t forget to be a good work colleague, friend, daughter/ son, Mum, dad
- Try to get good sleep
- Don’t forget to live LOL
Its that simple that if you just keep going and just get it done it will ALL fall into place!
WRONG....!!!
We are not machines we are human beings that our governed by our EMOTIONS and OUR LEARNED EXPERIENCES.
If as a friend or practitioner or patient you are not present in the now or authentically listening and allowing the person to feel heard then it’s not that simple. Furthermore if you are not guiding or asking the “right” questions bridge that gap then you or they may feel unheard and also resistant to change!
WRONG....!!!
We are not machines we are human beings that our governed by our EMOTIONS and OUR LEARNED EXPERIENCES.
If as a friend or practitioner or patient you are not present in the now or authentically listening and allowing the person to feel heard then it’s not that simple. Furthermore if you are not guiding or asking the “right” questions bridge that gap then you or they may feel unheard and also resistant to change!
“On the path to change resistance will be encountered”
Their are many types of resistance to change that exits and it can either be covert or overt, organized or individual.
More often then not a person can be resistant to change when they perceive that the change that is occurring is a threat to them.
Those who encounter resistance to change from the people they work with may say stories such as this:
Behavioural analysts would call this type of explanation, explainatory fiction, which they would agrue is an inadequate. As this does not explain what function this behaviour serves nor why this person is behaviouring the way they are. This is a massiabe topic for another time... In short Resistance to change can also be noted in physiotherapy or personal training or coaching as:
Examples of psychological resistance which you may notice are attached to specific personality types:
Recognising whether they have any of these personality characteristics combined with assessing their readiness for change (sel below) can be a game changer to your practice:
More often then not a person can be resistant to change when they perceive that the change that is occurring is a threat to them.
Those who encounter resistance to change from the people they work with may say stories such as this:
- “I’ve tried everything with my patient /client friend and no matter what nothings changing!”
- “He/she is not putting in the work”
- “They don’t want the change enough”
- “They are not ready for the change”
- “They are lazy”
- “This person is becoming too much hard work, they require too much reassurance and hand holding”
- “They are not taking ownership of their condition! Evidence clearly shows exercise helps improve heath markers, lower back pain suffers and they still wont do anything”
Behavioural analysts would call this type of explanation, explainatory fiction, which they would agrue is an inadequate. As this does not explain what function this behaviour serves nor why this person is behaviouring the way they are. This is a massiabe topic for another time... In short Resistance to change can also be noted in physiotherapy or personal training or coaching as:
- Non compliance
- Inconsistent
- Defensive
- No acceptance
- Avoidant and the list could go on...
Examples of psychological resistance which you may notice are attached to specific personality types:
- perfectionism
- criticising others
- self-critical
- preoccupied with appearance social withdrawal, need to be seen as independent and invulnerable
- inability to accept compliments or constructive criticism
Recognising whether they have any of these personality characteristics combined with assessing their readiness for change (sel below) can be a game changer to your practice:
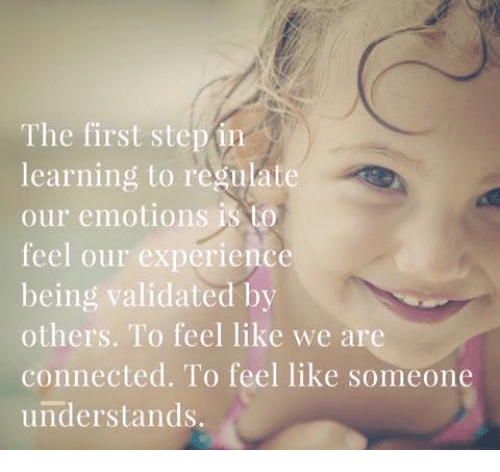
In fact John Bowbly a British psychiatrist first coined the term Attachment theory as a result of the studies he conducted to understand the developmental psychology of children. Bowlby who also worked with Ainsworth described attachment as a “deep and enduring emotional bond that connects one person to another across time and space”
His theory states their is a need for a strong emotional and physical attachment/ bond to at least one primary caregiver (mother, father etc) to aid a child’s personal development.
His theory states their is a need for a strong emotional and physical attachment/ bond to at least one primary caregiver (mother, father etc) to aid a child’s personal development.
Other psychologists also contributed to his work that argued attachment is a set of learned behaviors. This tied in with the evolutionary theory of attachment which suggests that children come into the world biologically / genetically pre-programmed to form attachments with others, because this will help them to survive. In fact the first few hours/ days are critical to the child's ability to imprint on another so they are able to form this attachment.
As the child develops later on in life they may go on to develop either one of these attachment personality types;
Poor development can cause a child who becomes an adult to develop and carry
Why is this or why should this be relevant when it comes to being a doctor / personal trainer/ coach / physiotherapist / osteopath?
If a patient has poor resiliency for instance they may be less likely to manager their flare ups well
Understanding your clients perdispositions and stage of readiness is necessary if you are going to embark advocating change.
Another reason why you may encounter resistance to change is:
Don’t freak out don’t beat yourself up!
Their is always another way :)
Want to know more? click here for part two....
References
Pending...
As the child develops later on in life they may go on to develop either one of these attachment personality types;
- Secure attachment style - autonomous
- Dismissive/ avoidant attachment style
- Pre-occupied/ anxious attachment style
- Disorganised/ unresolved attachment style
Poor development can cause a child who becomes an adult to develop and carry
- Poor understanding of what emotions they are feeling
- Inability to Regulate their emotions
- Poor Resiliency / bounce back ability
Why is this or why should this be relevant when it comes to being a doctor / personal trainer/ coach / physiotherapist / osteopath?
If a patient has poor resiliency for instance they may be less likely to manager their flare ups well
Understanding your clients perdispositions and stage of readiness is necessary if you are going to embark advocating change.
Another reason why you may encounter resistance to change is:
- You don’t know what your expectations or their (clients/ patients) expectations are
- You haven’t managed yours or your clients/ patients expectations.
- You wasn’t present to pay attention to what you are feeling or what your patient / client is telling you
- You havent regconised that your client may need to learn healthy coping strategies for self management
Don’t freak out don’t beat yourself up!
Their is always another way :)
Want to know more? click here for part two....
References
Pending...
Author
Sevda Onder
Nearly 20 years in the health and fitness industry.
Less than 10 years of post graduate physiotherapy experience.
£150 initial assessment
Physiotherapy 6/12 pack paid up front 15% off
Note I do offer low income slots for those who cannot afford my prices.
Please do not hesitate to reach out [email protected].
Less than 10 years of post graduate physiotherapy experience.
£150 initial assessment
Physiotherapy 6/12 pack paid up front 15% off
Note I do offer low income slots for those who cannot afford my prices.
Please do not hesitate to reach out [email protected].



 RSS Feed
RSS Feed